Death remains a mysterious and often uncomfortable topic for many. Over time, people have sought to make sense of and predict the end of life. Interestingly, scientific studies suggest that our sense of smell might offer insights into the nearness of death. Research indicates that our noses can provide subtle hints about when someone might be close to dying — not only by detecting scents associated with others’ deaths but also through the decline in our own sense of smell, which may signal future health issues.

One fascinating aspect of our sense of smell is its possible ability to detect when someone is nearing death. There are numerous personal accounts from people who say they noticed a distinct smell just before a loved one passed away. These stories suggest the presence of a mysterious sixth sense connected to our olfactory system. Several theories try to explain this phenomenon. One proposes that as a person nears death, the body releases specific chemicals or scents that, while undetectable to most, can be picked up by individuals with an especially sensitive sense of smell.
Another theory links this perception to emotional awareness, suggesting that subtle changes in our emotional environment may trigger a sensory reaction. In this view, it’s not that we consciously smell death, but rather that our sense of smell helps us intuitively recognize its approach.
Although scientific research in this field is still limited, a few intriguing studies have been carried out. One study by researchers at the University of Chicago revealed that animals—such as dogs and even cats—can detect chemical changes in people suffering from certain medical conditions, including cancer. This raises the possibility that humans with an especially keen sense of smell might also be able to perceive signs that death is near. There are also documented cases of animals living in hospitals and long-term care facilities that seem to consistently and accurately anticipate when a patient or resident is about to die.
In addition to detecting death in others, losing your sense of smell could also be a sign of future health problems. Studies have shown that a decline in the ability to smell may be linked to serious conditions like Parkinson’s and Alzheimer’s disease.
It can also be connected to issues with the heart and lungs. The sense of smell often weakens before other symptoms of these illnesses appear, which means it could act as an early warning sign. This can help people and doctors catch health problems sooner and take action earlier.
One study, published in the Journal of the American Geriatrics Society, found that older adults with a poor sense of smell were more likely to die within five years compared to those with normal smell function. This shows that losing your sense of smell might be a strong clue about your overall health and risk of death, giving doctors a helpful tool for early care and prevention.
As we learn more about the human body, we’re finding new ways that our senses and systems work together. The sense of smell, which is often ignored compared to sight or hearing, shows promise in helping us predict when death is near in others and in identifying future health risks. More research is needed to confirm these findings. Scientists are studying the chemical changes that happen in the body before death and how problems with smell relate to overall health and the risk of death. With better knowledge, we might be able to create tools that use smell to help people get early and important medical care.
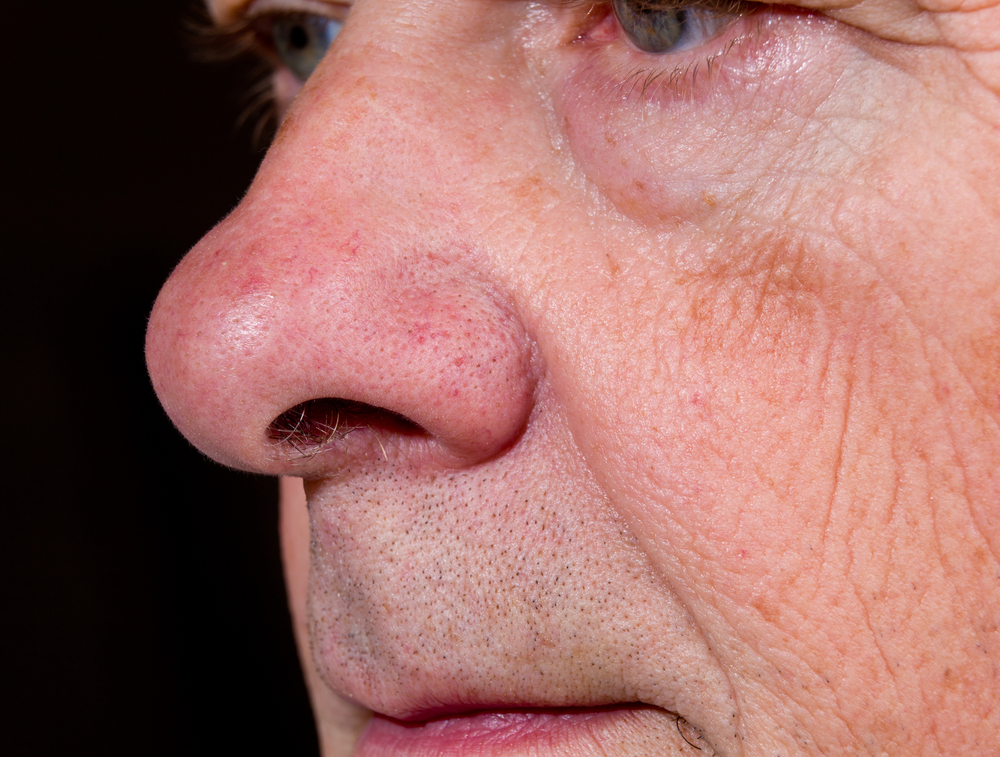
The idea that “the body senses when death is near, starting with the nose” is a captivating subject for research. Both the ability to detect death in others through smell and the loss of smell as a sign of future health issues offer exciting new directions for medicine and biology. By studying and using our sense of smell, we could gain important knowledge about life and death, helping to enhance overall health and well-being.
Recognizing the signs and symptoms of the end-of-life stage is important for caregivers and family members to offer the right physical, emotional, and spiritual support. This knowledge can reduce anxiety, create meaningful moments, and help ensure comfort during this significant time.
Being aware of end-of-life symptoms in older adults helps you better understand what your loved one may be going through and makes the transition smoother and more compassionate for everyone.
Caring for someone in their final stage of life is very challenging. Whether you are the main caregiver or just helping out, it’s normal to wonder what to expect. Knowing the physical, emotional, and mental changes that happen can guide you in providing comfort and reassurance during this deeply meaningful time.
Every person’s end-of-life journey is different, and signs won’t always appear in the same order or with the same intensity. This timeline is meant as a general guide, but experiences can vary widely from one individual to another. The speed of these changes can also differ—some may show obvious physical signs, while others may have more subtle ones. Below is an overview of what you might notice during the weeks, days, and hours before the end of life.
In the weeks before the end of life, your loved one may start to pull away from daily activities. These changes can be both emotional and physical.
Emotional Changes:
- A feeling of acceptance or detachment from the world.
- Low mood, less motivation, and less interest in hobbies or socializing.
- More time spent thinking about childhood or past memories.
Physical Changes:
- Loss of appetite and less interest in eating.
- Noticeable weight loss and becoming more fragile.
- Growing weakness and tiredness.
During this time, it’s important to offer gentle support. Avoid forcing them to eat or join activities they don’t want to. Instead, create a calm and peaceful space where they feel safe and comfortable.
As the end approaches, changes become more noticeable. Your loved one may sleep most of the time and might not respond much when awake.
Physical Signs:
- Sleeping more often.
- Moving less and having a limited response to talking or touch.
- Breathing may become harder or irregular.
- Difficulty swallowing or refusing food and drinks.
- Little to no bowel movements or urination.
Emotional and Mental Signs:
- Seeing or hearing things that aren’t there (hallucinations, illusions, or delusions).
- Growing confusion and feeling disoriented.
- Restlessness or brief moments of sudden energy.
Keep talking to your loved one gently and lovingly, even if they don’t seem to respond. It’s believed they can still hear you until the very end.
In the last hours, the body gradually starts to shut down, and vital functions slow down considerably.
Physical Signs:
- Breathing becomes irregular, with pauses known as apnea.
- Noisy breathing or a “death rattle” caused by fluid in the throat.
- Eyes may appear glassy and unfocused.
- Hands and feet feel cold, and skin may change color, showing blotchy patterns (mottling).
- Pulse becomes weak or may not be felt at all.
Emotional Signs:
- Brief moments of alertness or waking up.
- Changes in awareness, including confusion, delirium, or unresponsiveness.
During this time, family and caregivers should focus on creating a peaceful and loving environment. Hold their hand, speak gently, and offer comforting words.
When death happens, the body relaxes completely, and all vital signs come to a stop.
Signs of Death:
- Breathing stops.
- No pulse or heartbeat can be detected.
- Pupils widen and do not respond to light.
- Skin looks pale and waxy.
- There may be small, automatic movements or tears.
After death, take time to sit quietly with your loved one, reflect, and say your goodbyes. Allow yourself to feel and process your emotions without judgment. You might find comfort in talking with close friends or family, reaching out to a grief counselor, or joining support groups for those who are grieving. Handling practical matters like informing others, arranging care for the body, and planning funeral services can also help provide focus during this difficult time. Remember, grief is a personal experience, and it’s normal to feel a wide range of emotions.
Below are detailed explanations of common end-of-life symptoms, along with ways to respond with care and compassion.
1. Changes in Appetite and Digestion
As the body begins to shut down, metabolism slows down a lot. This causes less hunger and thirst.
What to Expect:
- Decreased appetite and less interest in eating.
- Trouble swallowing food or liquids.
- Feeling nauseous or experiencing constipation.
How to Help:
- Offer small amounts of their favorite foods.
- Give ice chips or use a damp cloth to keep their lips moist.
- Don’t force them to eat or drink if they’re not interested.
2. Increased Sleep
In the last weeks and days, fatigue and weakness grow much stronger, causing your loved one to sleep more.
What to Expect:
- Longer periods of sleep.
- Harder to wake them up.
How to Help:
- Let them rest as much as they need.
- Speak quietly and offer gentle touches for comfort.
3. Withdrawal from the World
It’s normal for your loved one to become emotionally distant and less engaged with their surroundings.
What to Expect:
- Less interest in social activities.
- More focus on memories or personal reflection.
How to Help:
- Be there for them without pushing them to join in.
- Create a calm and peaceful space.
4. Anxiety and Depression
Emotional struggles like anxiety or depression are common. Caregivers may benefit from professional help such as therapists, grief counselors, or support groups focused on end-of-life care. Many hospice programs also provide counseling and resources for both patients and caregivers. Remember to practice self-care, set limits, and take time to rest and reflect to maintain your own emotional health during this difficult time.
What to Expect:
- Feelings of fear or anxiety about what’s ahead.
- Sadness or feelings of regret.
How to Help:
- Encourage honest and open talks.
- Provide comfort and reassurance.
5. Loss of Control Over Urine and Bowels
Muscle control weakens, leading to incontinence.
What to Expect:
- Less urine production.
- Loss of control over bowel movements.
How to Help:
- Use incontinence products as needed.
- Keep the skin clean and dry to prevent discomfort.
6. Changing Vital Signs
Blood pressure, heart rate, and body temperature often decrease.
What to Expect:
- Hands and feet may feel cool to the touch.
What to Expect:
- Skin may develop blotchy, purple or blue patches (mottling).
How to Help:
- Keep your loved one warm with blankets.
- Be careful not to let them get too hot.
7. Confusion
Cognitive decline often occurs near the end of life.
What to Expect:
- Disorientation and confusion.
- Talking to people who aren’t there.
How to Help:
- Stay calm and provide gentle reassurance.
- Avoid correcting or arguing with them.
8. Sensory Changes
Changes in vision and hearing are common.
What to Expect:
- Seeing or hearing things that aren’t there (hallucinations).
- Talking to people who aren’t present.
How to Help:
- Allow them to share their experiences without dismissing or arguing.
9. Saying Goodbye
Many people want to resolve unfinished business before they pass.
What to Expect:
- Meaningful final conversations.
- Discussions about funeral arrangements.
How to Help:
- Honor and support their wishes.
- Listen with kindness and understanding.
10. Breathing Changes
Breathing may slow down and become uneven.
What to Expect:
- Shallow, irregular breaths.
- Noisy or rattling sounds while breathing.
How to Help:
- Keep their head and upper body slightly elevated.
- Use a humidifier to ease breathing.
11. Loss of Consciousness
Awareness gradually fades.
What to Expect:
- Becoming unresponsive.
- Eyes appearing glassy or vacant.
How to Help:
- Keep speaking softly to them.
- Hold their hand to offer comfort.
Providing Comfort and Support
End-of-life care is a deeply meaningful time. Showing compassion, patience, and simply being present will bring comfort to your loved one and peace to you during this final chapter.
Physical Comfort:
- Use a humidifier to ease breathing.
- Keep lips and skin moisturized.
- Frequently adjust their position to prevent discomfort.
Emotional Comfort:
- Speak gently and calmly.
- Play soothing music.
- Avoid dismissing or ignoring their thoughts and feelings.
Spiritual Comfort:
- Consider involving a spiritual advisor if desired.
- Respect their personal beliefs and rituals.
End-of-life care is a sacred and deeply emotional time, marking a significant chapter for both the person passing and their caregivers. This period is often filled with sorrow, love, reflection, and moments of peace. Caregiving during this time can be physically and emotionally demanding, making self-care and support essential.
Caring for someone in their final days goes beyond physical tasks—it’s about creating an environment full of dignity, respect, and love. Simple gestures like holding their hand, speaking softly, or playing their favorite music can bring great comfort. These small acts have a profound impact on both the person at the end of life and those who care for them.
Self-care for caregivers is not a luxury—it’s essential. Burnout, exhaustion, and emotional overwhelm are very real risks during this time. Taking regular breaks, asking for help from friends, family, or professional caregivers, and setting aside moments for personal reflection are crucial for maintaining your strength and resilience. Support groups, grief counselors, and hospice services can also provide valuable guidance and emotional support.
Grief after a loss is a deeply personal process with no fixed timeline. It’s normal to experience a wide range of emotions—anger, guilt, sadness, relief, or numbness. All of these feelings are valid, and allowing yourself to experience them without judgment is important for healing.
As you move through this journey, remember that the love, patience, and care you’ve given are priceless. You have provided your loved one with an extraordinary gift: your presence, compassion, and dignity during their final moments. Ultimately, the memories of these shared times, even when difficult, often become treasured reflections of love and connection.
End-of-life care is not just about managing symptoms; it’s about honoring the person, their legacy, and the relationships they have built. By caring for your loved one while also caring for yourself, you can find moments of peace amidst the sorrow—knowing your presence truly made a meaningful difference in their last chapter.
- My Mother-in-Law Tried On My Wedding Dress and Destroyed It — So I Made Her Regret It Publicly
- He Cheated. She Laughed. I Served Them Both a Slideshow of Karma
- “I Overheard My Husband and Our Neighbor’s Daughter — So I Came Up With a Plan She Never Saw Coming”
- He Couldn’t Move, But He Knew Something Was Wrong — So He Looked Up
- I Gave a Ride to a Homeless Man — The Next Morning, Black SUVs Surrounded My Home
- I Married My Former Teacher — But Our Wedding Night Revealed a Secret I Never Saw Coming

